What is HbA1c ?
HbA1c is your average blood glucose (sugar) levels for the last two to three months. If you have diabetes, an ideal HbA1c level is 48mmol/mol (6.5%) or below.
What does HbA1c mean?
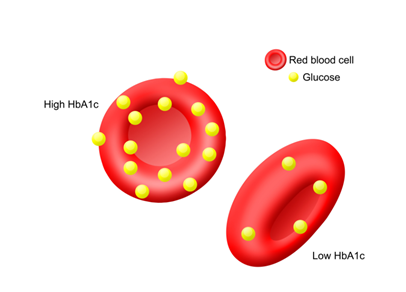
HbA1c is what’s known as glycated haemoglobin. This is something that’s made when the glucose (sugar) in your body sticks to your red blood cells. Your body can’t use the sugar properly, so more of it sticks to your blood cells and builds up in your blood. Red blood cells are active for around 2-3 months, which is why the reading oh HbA1c is taken quarterly.
A high HbA1c means you have too much sugar in your blood. This means you’re more likely to develop diabetes complications.
People who have diabetes need this test regularly to see if their levels are staying within range. It can tell if you need to adjust your diabetes medicines.
What Is Hemoglobin?
Hemoglobin is a protein found in red blood cells. It gives blood its red color, and its job is to carry oxygen throughout your body.
What is a HbA1c test?
The hemoglobin A1c (HbA1c) test measures the amount of blood sugar (glucose) attached to your hemoglobin. It is an important blood test that gives a good indication of how well your diabetes is being controlled. Most people will have the test every three to six months.
Few people needs this test often like in pregnancy And some people will need the test less often, usually with controlled blood glucose levels.
An HbA1c test is also used to diagnose diabetes, and to keep an eye on your levels if you’re at risk of developing diabetes (you have prediabetes). The test is sometimes called haemoglobin A1c or just A1c.
How the Test Works
The sugar in your blood is called glucose. When glucose builds up in your blood, it binds to the hemoglobin in your red blood cells. The A1c test measures how much glucose is bound.
Red blood cells live for about 3 months, so the test shows the average level of glucose in your blood for the past 3 months. If your glucose levels have been high over recent weeks, your hemoglobin A1c test will be higher
Your HbA1c results
You should get the results quickly. The result of this test lets your healthcare team know if they need to change your treatment or medication to help you manage your levels better.
And your HbA1c can change for lots of reasons, including:
- if you’re unwell
- if you’re taking other medicines, like steroids
- changes in lifestyle
- if you’re feeling very stressed or you’re depressed.
Diagnosing Prediabetes or Diabetes
| Normal | Below 5.7% |
|---|---|
| Prediabetes | 5.7% to 6.4% |
| Diabetes | 6.5% or above |
What is a normal range for an HbA1c test ?
If you have diabetes, an ideal HbA1c level is 6.5% or below.
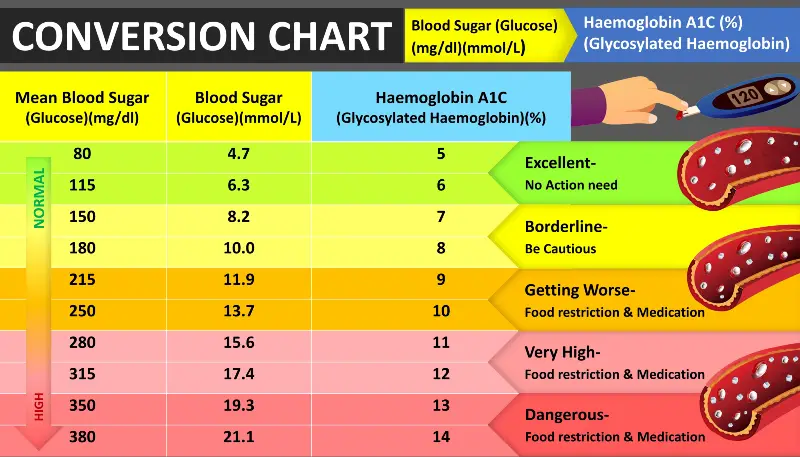
What should be the normal range if we are at risk of developing diabetes ?
There are different target HbA1c levels for people at risk of developing type 2 diabetes. If you’ve been told you’re at risk, your target level should be below 6%.
Why would I need this test ?
The test for HbA1c is used to diagnose and monitor diabetes. For people who have diabetes, the test is used to indicate how well the diabetes has been controlled over the last few months. People with diabetes are advised to have this test every 3 to 6 months, or more frequently if it is not under control. This is important. The higher the HbA1c, the greater the risk of developing complications such as problems with your eyes and kidneys.
Who Should Get an A1C Test, and When?
Testing for diabetes or prediabetes:
Get a baseline A1C test if you’re an adult over age 45—or if you’re under 45, are overweight, and have one or more risk factors for prediabetes or type 2 diabetes:
- If your result is normal but you’re over 45, have risk factors, or have ever had gestational diabetes, repeat the A1C test every 3 years.
- If your result shows you have prediabetes, talk to your doctor about taking steps now to improve your health and lower your risk for type 2 diabetes. Repeat the A1C test as often as your doctor recommends, usually every 1 to 2 years.
- If you don’t have symptoms but your result shows you have prediabetes or diabetes, get a second test on a different day to confirm the result.
Understanding your results
If you have not previously been diagnosed as having diabetes, an HbA1c of 6.5% or more can indicate that you do have diabetes. And if your level is lower than this, you might need other tests to check whether you have diabetes or not.
If you do have diabetes, your doctor will usually aim for an HbA1c of 6.5-7%. And If the HbA1c is higher than the target range, your doctor may consider changing your treatment or closer monitoring.
There are some medical conditions, such as anaemia, that change red blood cells and affect your HbA1c result.
How to lower your HbA1c levels
If your levels have gone above your target since your last check, it’s understandable to be worried. Even a slightly high HbA1c level puts you more at risk of developing serious complications in your body. But knowing your numbers and what that means is an important and good first step – now you need to know how to lower them.
- Your Doctor may need to review your medication and increase the dose or try a new one.
- Get more active – moving more is good for everyone, but it can specifically help to bring down your HbA1c levels.
- Consult your Dietitian/ Nutritionist get advice on balanced, healthy eating.
- Stop smoking – smoking makes it harder for blood to flow around your body.
Management
Keeping your blood sugar levels within the range recommended by your doctor or Dietitian can be challenging. That’s because many things make your blood sugar levels change, sometimes unexpectedly. Following are some factors that can affect your blood sugar levels.
1. Food

Healthy eating is a corner stone of healthy living — with or without diabetes. But if you have diabetes or elevated sugar level , you need to know how foods affect your blood sugar levels. It’s not only the type of food you eat, but also how much you eat and the combinations of food types you eat.
What to do:
- Learn about carbohydrate counting and portion sizes. A key to many diabetes management plans is learning how to count carbohydrates. Carbohydrates often have the biggest impact on your blood sugar levels .Learn what portion size is appropriate for each food type. Simplify your meal planning by writing down portions for foods you eat often. Use measuring cups or a scale to ensure proper portion size and an accurate carbohydrate count.
- Make every meal well balanced. As much as possible, plan for every meal to have a good mix of starches, fruits and vegetables, proteins, and fats. Pay attention to the types of carbohydrates you choose. Some carbohydrates, such as fruits, vegetables and whole grains, are better for you than others. These foods are low in carbohydrates and have fiber that helps keep your blood sugar levels more stable.
- Coordinate your meals and medications. Too little food in proportion to your diabetes medications — especially insulin — may result in dangerously low blood sugar (hypoglycemia). Too much food may cause your blood sugar level to climb too high (hyperglycemia). Talk to your diabetes health care team about how to best coordinate meal and medication schedules.
- Avoid sugar-sweetened beverages. Sugar-sweetened beverages tend to be high in calories and offer little nutrition. And because they cause blood sugar to rise quickly, it’s best to avoid these types of drinks if you have diabetes.
2. Exercise

Physical activity is another important part of your diabetes management plan. When you exercise, your muscles use sugar (glucose) for energy. Regular physical activity also helps your body use insulin more efficiently. These factors work together to lower your blood sugar level. The more strenuous your workout, the longer the effect lasts. But even light activities — such as housework, gardening or being on your feet for extended periods — can improve your blood sugar.
What to do:
- Talk to your doctor about an exercise plan. Ask your doctor about what type of exercise is appropriate for you. In general, most adults should get at least 150 minutes a week of moderate aerobic activity. Aim for about 30 minutes of moderate aerobic activity a day on most days of the week.If you’ve been inactive for a long time, your doctor may want to check your overall health before advising you. He or she can recommend the right balance of aerobic and muscle-strengthening exercise.
- Keep an exercise schedule. Talk to your doctor about the best time of day for you to exercise so that your workout routine is coordinated with your meal and medication schedules.
- Stay hydrated. Drink plenty of water or other fluids while exercising because dehydration can affect blood sugar levels.
- Be prepared. Always have a small snack or glucose tablets with you during exercise in case your blood sugar level drops too low. Wear a medical identification bracelet.
3. Alcohol

The liver normally releases stored sugar to counteract falling blood sugar levels. But if your liver is busy metabolizing alcohol, your blood sugar level may not get the boost it needs from your liver. Alcohol can result in low blood sugar shortly after you drink it and for as long as 24 hours afterward.
What to do:
- Get your doctor’s OK to drink alcohol. Alcohol can aggravate diabetes complications, such as nerve damage and eye disease. But if your diabetes is under control and your doctor agrees, an occasional alcoholic drink is fine.Moderate alcohol consumption is defined as no more than one drink a day for women of any age and men over 65 years old and two drinks a day for men under 65. One drink equals a 12-ounce beer, 5 ounces of wine or 1.5 ounces of distilled spirits.
- Don’t drink alcoholic beverages on an empty stomach. If you take insulin or other diabetes medications, be sure to eat before you drink, or drink with a meal to prevent low blood sugar.
- Check your blood sugar level before bed. Because alcohol can lower blood sugar levels long after you’ve had your last drink, check your blood sugar level before you go to sleep. If your blood sugar isn’t between 100 and 140 mg/dL (5.6 and 7.8 mmol/L), have a snack before bed to counter a drop in your blood sugar level.
4. Menopause
Changes in hormone levels the week before and during menstruation can result in significant fluctuations in blood sugar levels.
What to do:
- Look for patterns. Keep careful track of your blood sugar readings from month to month. You may be able to predict fluctuations related to your menstrual cycle.
- Check blood sugar more frequently. If you’re likely approaching menopause or experiencing menopause, talk to your doctor about whether you need to monitor your blood sugar level more often. Symptoms of menopause can sometimes be confused with symptoms of low blood sugar, so whenever possible, check your blood sugar before treating a suspected low to confirm the low blood sugar level.
Most forms of birth control can be used by women with diabetes without a problem. However, oral contraceptives may raise blood sugar levels in some women.
5. Stress

If you’re stressed, the hormones your body produces in response to prolonged stress may cause a rise in your blood sugar level. Additionally, it may be harder to closely follow your usual diabetes management routine if you’re under a lot of extra pressure.
What to do:
- Look for patterns. Log your stress level on a scale of 1 to 10 each time you log your blood sugar level. A pattern may soon emerge.
- Take control. Once you know how stress affects your blood sugar level, fight back. Learn relaxation techniques, prioritize your tasks and set limits. Whenever possible, avoid common stressors. Exercise can often help relieve stress and lower your blood sugar level.
- Get help. Learn new strategies for coping with stress. You may find that working with a psychologist or clinical social worker can help you identify stressors, solve stressful problems or learn new coping skills.
If you’re having trouble keeping your blood sugar level in your target range, ask your Medico and para medico health care team for help.
For more information click here
If you are struggling shedding weight. You can talk to us by taking this assessment: Click here

