What is PCOS?
PCOS stands for Polycystic Ovarian Syndrome which is a form of hormonal imbalance that affects 1/10 women of reproductive age, in India, today. The syndrome leads to overproduction of male hormones in women, resulting in multiple surfaced/under-surfaced symptoms.
Studies suggest that up to 70 percent of women with PCOS hadn’t been diagnosed. Underdiagnoses results in delay in seeking help therefore worsening the situation. Physically, PCOS affects a woman’s ovaries, resulting in disturbed production of estrogen and progesterone. The syndrome leads to other physical and mental effects on the overall wellbeing of the sufferer.
There are three main characteristics of PCOS:
- First one is the formation of cysts in the ovaries
- Second one is high level production of male hormones
- And the third one is irregular periods or absence of periods for longer periods.
Between 5% and 10% of women of reproductive age can have PCOS. Furthermore, mostly women find out that they have PCOS in their 20s and 30s, when they have problems getting pregnant. But everyone should know that PCOS can happen at any age after puberty.
What is the prevalence of PCOS in India?
The exact prevalence of PCOS is not known as the syndrome is not defined precisely. Prevalence of PCOS is highly variable ranging from 2.2% to 26% globally. In few Asian countries, prevalence figures are ranging from 2% to 7.5% in China and 6.3% in Srilanka.
There are few studies conducted in India. Studies done in South India and Maharashtra, prevalence of PCOS were reported as 9.13% and 22.5% respectively.
[Source-https://www.nhp.gov.in/disease/endocrinal/ovaries/polycystic-ovary-syndrome-pcos]
Moreover, one in every 10 women in India has polycystic ovary syndrome (PCOS), among women of reproductive age, according to a study by PCOS Society. And out of every 10 women diagnosed with PCOS, six are teenage girls.
What is the difference between PCOD and PCOS?
- PCOD stands for polycystic ovarian disease and PCOS stands for polycystic ovarian syndrome.
- PCOS is a metabolic disorder which is a serious condition and PCOD is not considered a disease entirely.
- PCOD can be controlled with proper diet and also exercise routine. Whereas PCOS needs treatment by consulting doctors as it is a metabolic disorder (disruption in chemical processes of your body).
What are the symptoms of PCOS?
The symptoms of PCOS may include:
- Skipped periods, irregular periods, or very light periods
- Large ovaries or cysts in ovaries
- Excess body hair including the chest, stomach, and back
- Weight gain – obesity or overweight
- Acne or oily skin
- Male-pattern baldness or thinning hair/loss of scalp hair
- Infertility
- Dark or thick skin patches on the back of the neck, in the armpits, and under the breasts
What is the exact cause of PCOS?
The cause of PCOS is not perfectly clear. It is clear that genetic and environmental factors contribute to the development of PCOS. But do not know exactly what causes PCOS.
- Excess insulin production in your body: Insulin is the hormone produced in the pancreas that allows cells to use sugar. If your cells become resistant to the action of insulin, then your blood sugar levels can rise. In turn, your body might produce more insulin. Excess insulin might increase androgen production, causing difficulty with ovulation.
- Low-grade inflammation in your body: This term is describes white blood cells’ production of substances to fight infection. Research has shown that women with PCOS have a type of low-grade inflammation that stimulates polycystic ovaries to produce androgens. And it can also lead to heart and blood vessel problems.
- Heredity: Research suggests that certain genes might be linked to PCOS.
- Excess androgen production in the body: The ovaries produce abnormally high levels of androgen, resulting in hirsutism and acne.
(Source – https://www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439 )
Who is at risk of developing PCOS?
- Women of all races and ethnicities are at risk of PCOS.
- Your risk of PCOS may be higher if you have obesity or if you have a relative with PCOS.
- You may also be more likely to have it if you have insulin resistance.
How to detect that you have PCOS?
There’s no specific single test for PCOS but a physical exam, ultrasound, and blood tests can help in the diagnosis of PCOS.
The diagnosis begins with a thorough history and physical examination also. The main focus is on menstrual history, any fluctuations in the weight and their impact on PCOS symptoms, and also other PCOS-related symptoms.
A diagnosis of PCOS can be made if you have been ruled out of other rare causes of the same symptoms. And you meet at least 2 of the following 3 criteria:
- If you have irregular periods or no periods – this indicates that your ovaries do not regularly release eggs. In other words, ovulation occurs irregularly.
- If your blood tests show that you have high levels of such as androgen (or sometimes just the signs of excess male hormones, even if the blood test is normal).
- Also, your ultrasound scans show that you have polycystic ovaries.
Collections of 12 or more “cysts” on your ovaries that may be larger than normal also indicates PCOS. But women who don’t have PCOS may also have cysts, but fewer than 12 don’t meet the criteria for a diagnosis.

Diagnosis of polycystic ovary syndrome.
(CT = computed tomography; DHEA-S = dehydroepiandrosterone sulfate; FSH = follicle-stimulating hormone; LH = luteinizing hormone; MRI = magnetic resonance imaging; OGTT = oral glucose tolerance test; PCOS = polycystic ovary syndrome; TSH = thyroid-stimulating hormone.) (Source-https://www.aafp.org/afp/2016/0715/p106.html )
How to detect PCOS in adolescents?
Generally, it is difficult to diagnose PCOS in adolescent women. Especially, at an early stage during their first few years of menstrual cycle. In the beginning, menstrual cycles of adolescent women can be irregular for reasons that are unrelated to PCOS. Because in the first year, periods are often irregular, and in their second year periods, they normally settle into a regular pattern.
In adolescent women having PCOS, periods are either very close together (fewer than 21 days) or far apart (more than 45 days). And also if this irregularity continues after three years, this suggests PCOS might be the cause.
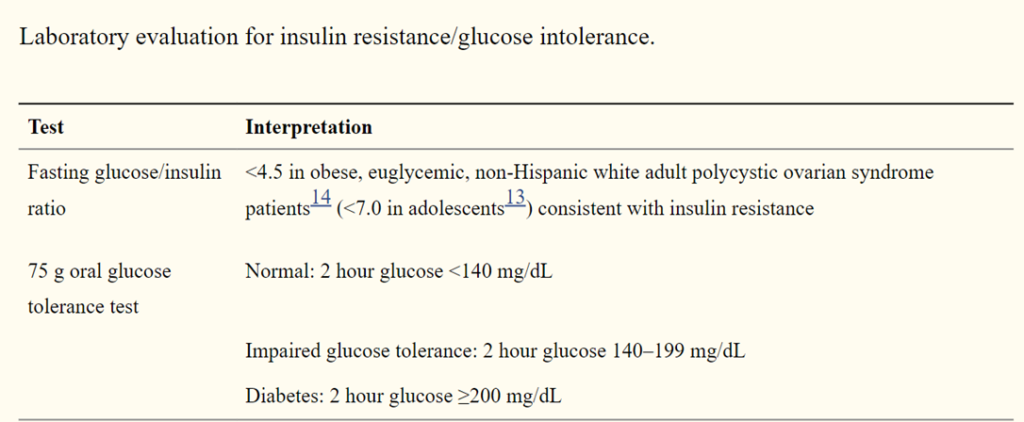
How to read these lab reports yourself at home?
Lab results are often shown as a set of numbers known as a reference range. A reference range may also be called normal values which are based on the normal test results of a large group of healthy people.
Your lab results may also include one of these terms:
- Negative or normal, which means the disease or substance being tested was not found.
- Positive or abnormal, which means the disease or substance was found.
- Inconclusive or uncertain, which means there wasn’t enough information in the results to diagnose or rule out a disease.
These are the reference range values for some of the tests that are conducted for the PCOS. These values might differ based on the type of method used in the laboratory.
Testosterone:
- Most testosterone values in PCOS will be ≤150 ng/dL (≤5.2 nmol/L).
- Testosterone values of ≥200 ng/dL (≥6.9 nmol/L) warrant consideration of an ovarian or adrenal tumor.
Dehydroepiandrosterone-sulfate (DHEA-S)
- DHEA-S values may be normal or slightly elevated in PCOS.
- Values ≥800 µg/dL (21.7 µmol/L) warrant consideration of an adrenal tumor.
17-hydroxyprogesterone
- A morning, fasting, unstimulated level of <200 ng/dL in the follicular phase reliably excludes late-onset 21-hydroxylase deficiency.
- Further evaluation of levels ≥200 ng/dL involves adrenocorticotropic hormone (ACTH)-stimulation with an intravenous 250 µg dose and a 30 minutes value (stimulated values ≥1,000 ng/dL confirm the diagnosis).
- Also, Oral contraceptives and glucocorticoids can affect values.
Luteinizing hormone/follicle stimulating hormone (LS/FSH) ratio
- A ratio ≥2.0 is suggestive of PCOS but is not highly sensitive or specific.
- Gonadotropin levels are affected by oral contraceptives.
(Source- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1069067/)
What are the health complications that developed due to PCOS?
Yes, studies have found links between PCOS and other health problems, including:
- Diabetes: One of the most common complications of PCOS is diabetes. According to researchers, more than half of women with PCOS will have diabetes or prediabetes before the age of 40.
- High blood pressure: Another complication is high blood pressure or hypertension. Women with PCOS are at greater risk of having high blood pressure compared with women of the same age without PCOS.
- High cholesterol: Women with PCOS often have higher levels of LDL cholesterol also known as bad cholesterol. And low levels of HDL (good) cholesterol which raises risk for heart diseases.
- Sleep apnea: A sleep disorder in an disorder in which breathing repeatedly stops and starts. Many women with PCOS are overweight or obesity, which can cause sleep apnea which raises the risk of heart disease and also diabetes.
- Depression and anxiety: Depression and anxiety are common among women with PCOS.
- Endometrial cancer: Anovulation, obesity, insulin resistance, and diabetes increase the risk of developing cancer of the endometrium.
What can you do to manage your PCOS?
PCOS can wreak havoc on your hormones and still doesn’t have a known cause and even permanent cure. Researchers suggest that the first line of treatment for PCOS is lifestyle changes, healthy diet and physical activity. This can also help women modify their focus and remove obstacles that may be in their way on the path towards wellness.
Lifestyle changes:
You can live with your PCOS without any complications if you change your lifestyle. There are certain things that I meant by a change in your lifestyle.
- For instance, weight loss if overweight or obese through a calorie deficit diet combined with moderate exercise activities. A modest reduction in your weight, per say, losing 5-10 percent of your body weight may improve your condition.
- Also, if you are taking any medications for your PCOS then losing weight may increase the effectiveness of medications.
- Regular sleep for about 7-8 hours is also essential for the management of PCOS. Sleep is important to our hormone health. If you’re not getting enough sleep, your body can’t repair itself. And also a good night’s sleep is essential for the physical and mental well-being of women.
Healthy diet:
What you eat plays an important role in the management of PCOS. The most important focus of diet is weight management. This helps in the regulation of hormone levels, which in turn helps to improve symptoms of PCOS.
When you combine a healthy diet with exercise, it is more effective than following only one thing alone in achieving a healthy weight. In the long term, a healthy diet aims not only to prevent weight gain. But also reduces the risk of related health conditions such as type 2 diabetes and cardiovascular disease.
1. Watch out for types of carbs you are eating:
Eat low glycemic index foods like whole grains, pulses and a variety of vegetables. Every day add them to your meals, to make sure that your body gets proper nutrition. These types of foods are also rich in fibre which makes them digest slowly and causes less glucose spikes in your body.
Some of the examples for low glycemic foods are whole grains and millets like wheat, oats, quinoa, jowar, bajra, ragi. Pulses and legumes like bengal gram dal (Chana dal), beans, rajma, peas. And vegetables like broccoli, cabbage, mustard leaves, etc are great to balance your hormones.
2. Reduce intake of milk and dairy products:
Milk and milk products are not completely prohibited for women with PCOS. You can consume milk and its products but in a limited amount. Excess consumption of dairy which is a carbohydrate can lead to an increase in blood glucose level. According to several reports, milk, nonfat in particular, can contribute to increased androgen and insulin levels.
You don’t need to completely eliminate dairy. You can consume a few servings per week unless you are a lactose intolerant.
3. Choose your fruits wisely:
There are certain fruits that are very high in natural sugar. If you are already insulin-resistant, then you need to watch out for what type of fruit you are consuming.
4. Include lean protein in your diet:
Eating meat low in fat will aid in weight loss and keep you feeling full longer.
Food sources: Salmon, tuna, shrimp, skinless chicken and turkey breast, beans, pulses, legumes, and tofu
5. Increase your intake of omega-3 fatty acid:
Fish oil is a rich source of omega-3 fatty acid. It is also associated with a long list of health benefits. There is some research indicating that omega-3 supplements can decrease androgen levels in women with PCOS.
Food sources: Cooking oil such as Olive oil, sunflower oil, safflower oil. And Nuts and oilseeds such as walnuts, almonds, chia seeds, flaxseeds, and sunflower seeds.
6. Choose food high in Vitamins and Minerals:
Various studies show that consuming foods high in Vitamin D, Vitamin B, and Magnesium will greatly aid in improving insulin resistance, and decrease the severity of symptoms associated with PCOS.
Vitamin D food sources: salmon fish, eggs, mushrooms and fortified products
Vitamin B food sources: eggs, meat such as chicken, tuna, mackerel, and salmon, and dark green vegetables, such as spinach and kale.
Magnesium food sources: Avocados, nuts and oilseeds, pulses, whole grains, banana
7. Do not skip meals:
Skipping meals can crash your blood sugar levels, leading to food cravings and overindulgence. Keeping a routine will allow your blood sugar levels to stabilize. Also, stable blood sugar aids in the proper androgen production in your body.
Best food for PCOS:
Physical activity and PCOS:
Exercise helps lower blood sugar levels. If you have PCOS, increasing your daily activity may help in improving insulin resistance. And also help you keep your weight under control. The best type of exercise is one that you’ll do regularly i.e. Aerobic exercise such as brisk walking, biking, swimming, and jogging.
The regular physical activity will help you to reduce androgens levels in your body. It will also improve insulin resistance, regulate menstrual cycles, improve fertility, improve self-esteem, reduce anxiety and depression. You can also see these improvements in your body even when weight loss doesn’t occur.
There are some of the exercise links for you which can help you in weight loss.
What foods to eat and what food to avoid in PCOS?
| Foods to eat | Foods to avoid |
Natural and unprocessed foods | Refined carbohydrates, such as mass-produced pastries and white bread |
| High fiber foods | Fried foods, such as fast food. |
| Lean meat salmon, tuna, sardines, and mackerel | Red meat, such as steaks, hamburgers, and pork. |
| Fresh fruits such as blueberries, blackberries, guava, kiwi and cherries. | Fruits such as sapota, banana, grapes, dates, raisins, litchi, etc. |
| Fresh vegetables such as kale, spinach, and other dark, leafy greens, broccoli, cabbage, etc. | |
| Whole grains such wheat, oats, quinoa, etc. | Sugary beverages, such as sodas and energy drinks. |
| Pulses and legumes such as dried beans, lentils, and other legumes | |
| Healthy fats such as olive oil, as well as avocados and coconuts, nuts, including pine nuts, walnuts, almonds, and pistachios. | Solid fats, including margarine, shortening, and lard. |
Counselling points:
- Firstly, eat regular meals including a variety of food groups.
- Also, include plenty of vegetables and salad (at least 5-6 servings every day).
- Include a good amount of protein and a low to moderate amount of carbohydrate in each meal.
- Opt for unrefined and unprocessed carbohydrates, such as whole grain cereals, legumes and fruit, rather than refined carbohydrates. (For example, white bread, white rice, soft drinks, lollipop, biscuits)
- Replace saturated fats with unsaturated fats such as olive oil, sunflower oil, safflower oil, mustard oil, palm oil, and soybean oil. Also, nuts and oilseeds such as walnuts, almonds, pumpkin seeds, sunflower seeds, sesame seeds, etc.
What is seed cycle and its role in PCOS?
Seed cycle is a naturopathic remedy which claims to balance hormones, boosts fertility, and ease symptoms of menopause. It has become a trend nowadays. This seed cycle involves eating flaxseeds, pumpkin seeds, sesame seeds, and sunflower seeds.
These seeds are taken in 2 phases.
First Phase: It instructs women to eat 1 tablespoon of freshly ground flax and pumpkin seeds. You have to take them everyday for the first 13–14 days of their menstrual cycle, which is known as the follicular phase.
Second Phase: During the second half of their cycle, which is known as the luteal phase, seed cyclers eat 1 tablespoon each of ground sunflower and sesame seeds per day until the first day of their next period when their cycle starts again.
Phase 1 is believed to support the estrogen-dominant follicular phase when the ovaries increase estrogen levels in the body. On the other hand, Phase 2 is believed to support the increase of progesterone in the luteal phase.
But there are no scientific proven reason behind these seed cycle.
What is the effect of Oral contraceptives pills (OCPs) in PCOS?
Oral contraceptive pills are estrogen and progesterone containing hormonal birth control pills that acts on a person’s monthly cycle.
Albeit considered the first-line therapy for PCOS, the data regarding the effects of this mode of treatment on metabolism of carbohydrates, lipids, insulin, coagulation, and inflammation profile in women with PCOS is conflicting.
In PCOS, oral contraceptives are used to improve clinical symptoms of overproduction of androgen. And also help in regulating the menstrual cycles. It protects the endometrium against effects of unopposed estrogen action. This happens because estrogen content in the OCP increases Sex Hormone Binding Globulin levels, thus decreasing the free circulating androgens. The progesterone in OCPs suppresses the secretion of Luteinizing Hormone and decreases androgen production. (Source- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6094524/)
OCPs may also reduce adrenal production of androgens.
Furthermore, use of OCPs in PCOS women should be individualized after risk stratification and not used if any contraindications exist.
If you are struggling shedding weight. You can talk to us by taking this assessment: Click here
For more information click here

