What is FODMAP?
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols.
FODMAPs are a group of sugars that are not completely digested or absorbed in your intestines. When these FODMAPs reach your small intestine, they move slowly, attracting water. When they pass into the large intestine, FODMAPs are fermented by gut bacteria, producing gas as a result. The extra gas and water cause the intestinal wall to stretch and expand. Because people with IBS have a highly sensitive gut, ‘stretching’ the intestinal wall causes exaggerated sensations of pain and discomfort.
FODMAPs are found naturally in many foods and food additives.
What is a low FODMAP diet?
A low Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols diet is the diet which is low in foods containing oligosaccharides, disaccharides, monosaccharides and polyols. The principle behind the diet is to give the gut a chance to heal, especially if you have gastrointestinal problems like IBS.
The treatment for people with IBS include avoiding high FODMAP foods and choosing low FODMAP foods as their daily staples. Also, it is important to monitor portion sizes because having a large amount of a low FODMAP food could turn it into a high FODMAP food.
Who should try this FODMAP diet?
Low FODMAP diets are for those people who suffer from digestive problems such as Irritable Bowel Syndrome (IBS). High FODMAP foods cause irritable bowel syndrome, but they also may aggravate IBS symptoms. That’s why a low FODMAP diet is often recommended for IBS treatment, Small intestinal bacterial overgrowth (SIBO) and also for functional GI disorders other than IBS.
How does the low FODMAP diet work?
Low FODMAP is a three-step elimination diet:
- Restriction: Firstly, stop eating high FODMAPs foods for a minimum of 6-8 weeks.
- Reintroduction: Once your stomach calms down, slowly reintroduce them one by one to see which ones are troublesome for you.
- Personalization: Once you identify the foods that cause IBS or any other digestive symptoms, you can avoid or limit them while enjoying everything else in your diet worry-free.
What happens when a person with IBS eats FODMAPs?
FODMAPs are found in a wide range of foods, and most people eat high FODMAP foods everyday without issue. When a person with GI problems or IBS eat FODMAPs, they move slowly through the small intestine attracting water. When they reach the large intestine, gut bacteria use the FODMAPs as a fuel source to survive. The bacteria rapidly ferment FODMAPs, producing gas as a result.
These events occur in all people i.e. people with and without IBS. The difference is that people with IBS can have problems with the speed at which contents move through the intestines or a highly sensitive gut wall as well. The extra water and gas in the intestines, causes the intestinal wall to stretch and expand and results in common IBS symptoms. These symptoms are pain, excessive wind, bloating, distension and altered bowel habit such as diarrhoea, constipation or both.
(Source- https://www.monashfodmap.com/about-fodmap-and-ibs/ )
What are the benefits of a low FODMAP diet?
A low FODMAP diet may help in improving the following symptoms:
- pain and discomfort
- bloating and distension
- Bowel habit such as diarrhea or constipation
- quality of life
You can see these benefits are usually within 2-6 weeks of following a low FODMAP diet.
In fact, the diet does not cure IBS symptoms, it just helps people to live more comfortably with their condition.
FODMAPs Guidelines:
- A diet low in FODMAPs may be an effective therapy in the management of GI symptoms in patients with IBS.
- The low FODMAPs diet limits foods that contain lactose, fructose, fructo-oligosaccharides (fructans), galacto-oligosaccharides (galactans), and polyols or sugar alcohols (sorbitol, xylitol, mannitol, isomaltase, and maltitol).
- A cutoff value for acceptable amounts of FODMAPs has not been well defined and is likely patient specific. Patients may tolerate small amounts, but symptoms can develop if they consume quantities that surpass their threshold.
- Nutrition intervention begins with elimination of all high FODMAPs foods from the diet for a trial period of 6 to 8 weeks.
- The challenge phase begins with a slow, controlled reintroduction of one FODMAPs diet category at a time to observe for symptoms and identify the most challenging foods.
- Nutritional deficiencies that can arise with the low FODMAPs diet include folate, thiamin, and vitamin B6 (from limiting cereals and breads), as well as calcium and vitamin D (from avoidance of dairy). The goal is to eventually reduce or eliminate GI symptoms, by creating a diet that includes FODMAPs at the most tolerable intake level, and with use of alternative foods.
- It does not present a cure but a dietary approach to improve symptoms and quality of life.
(Source – Krause’s Food & the nutrition care process, 14th edition)
A sample FODMAP diet plan:
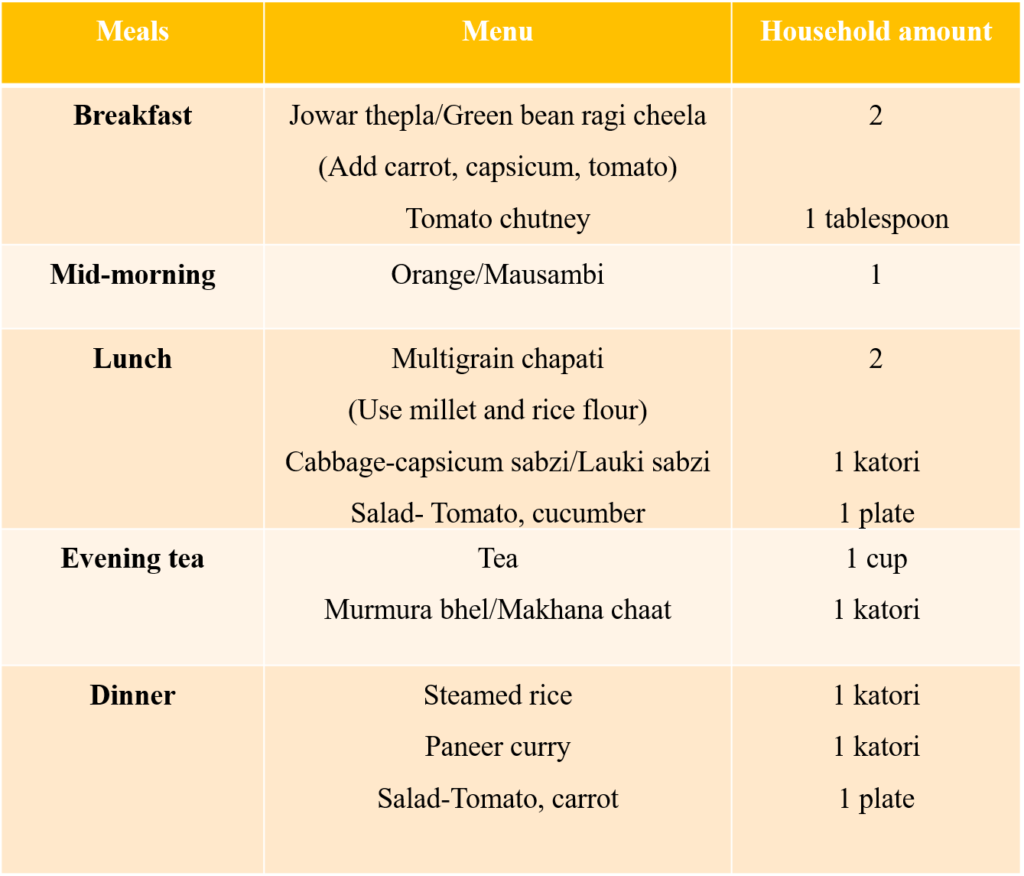
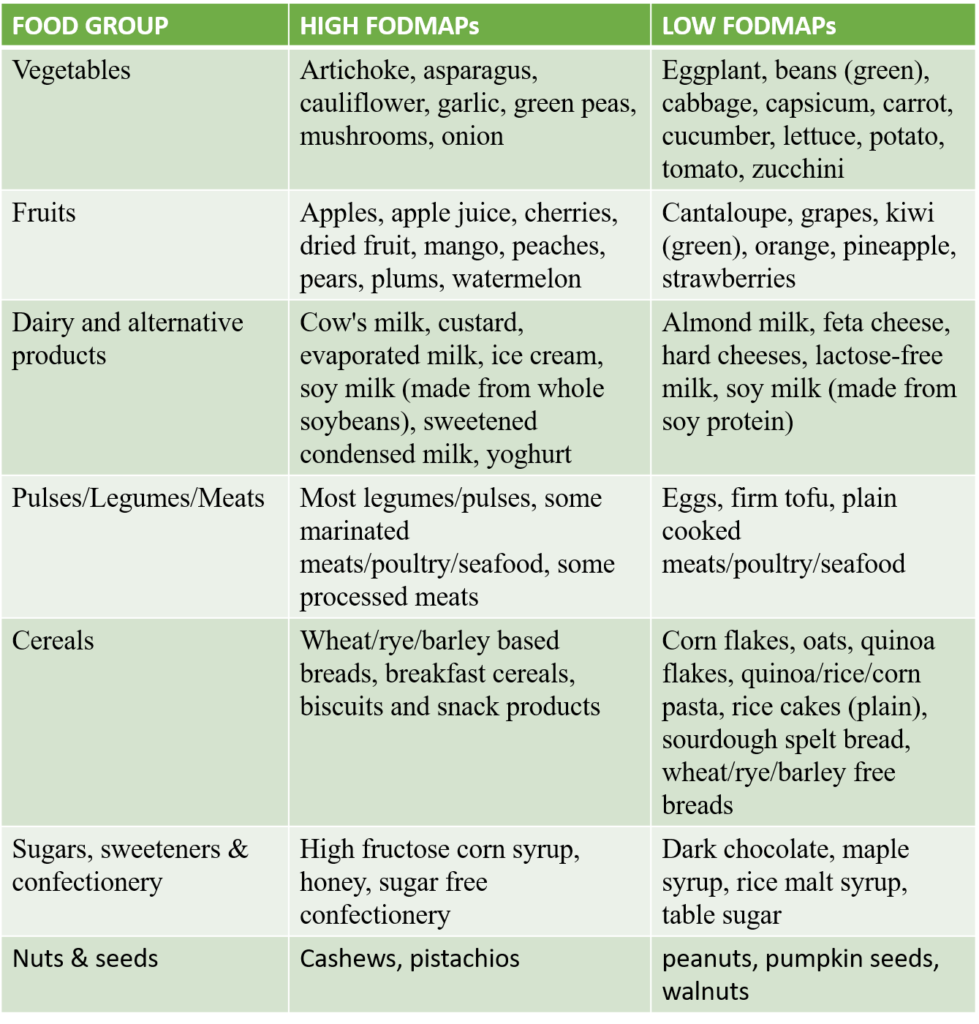
Table showing high FODMAPs and Low FODMAPs food sources:
To know more, have a look at the file below:
(Source- https://www.ibsdiets.org/fodmap-diet/fodmap-food-list/ )
If you are struggling shedding weight. You can talk to us by taking this assessment: Click here
For more information click here

