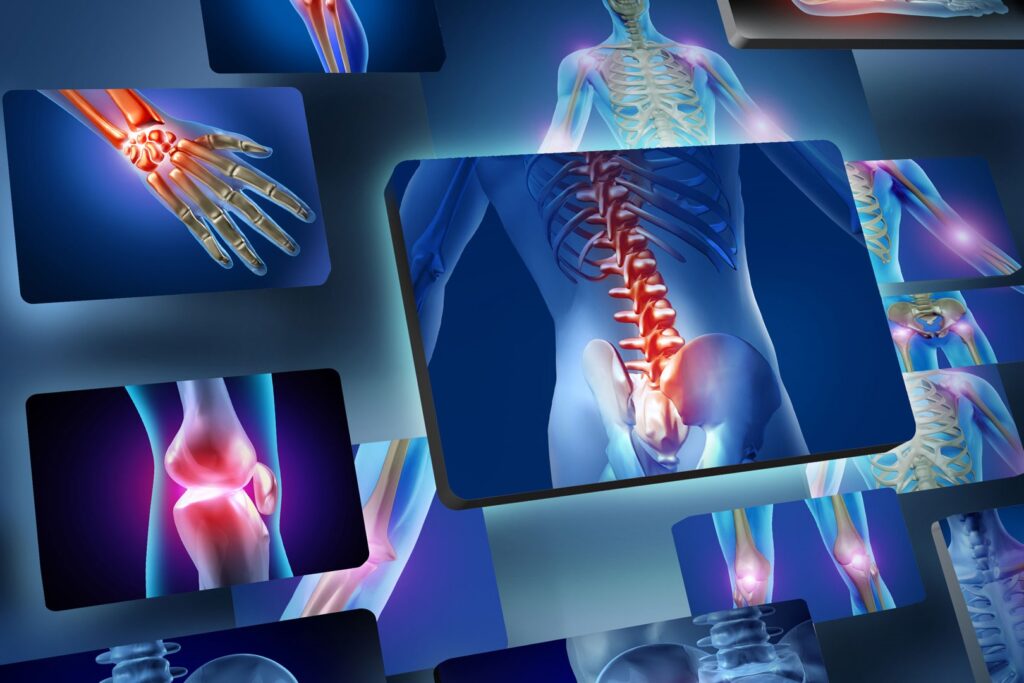
Rheumatoid arthritis (RA) causes joint inflammation and pain. It happens when the immune system doesn’t work properly and attacks the lining of the joints, called the synovium. The disease commonly affects the hands, knees or ankles, and usually the same joint on both sides of the body, such as both hands or both knees.
What is rheumatoid arthritis?
Rheumatoid arthritis (RA) is an autoimmune disease that is chronic (ongoing). It occurs in the joints on both sides of your body, which makes it different from other types of arthritis. You may have symptoms of pain and inflammation in your:
- Fingers
- Hands
- Wrists
- Knees
- Ankles
- Feet
- Toes
Uncontrolled inflammation damages cartilage, which normally acts as a “shock absorber” in your joints. In time, this can deform your joints. Eventually, your bone itself erodes. This can lead to the fusion of your joint (an effort of your body to protect itself from constant irritation).
Specific cells in your immune system (your body’s infection-fighting system) aid this process. These substances are produced in your joints but also circulate and cause symptoms throughout your body. In addition to affecting your joints, rheumatoid arthritis sometimes affects other parts of your body, including your:
- Skin.
- Eyes.
- Mouth.
- Lungs.
- Heart.
Age of onset of Disease
RA usually starts to develop between the ages of 30 and 60. But anyone can develop rheumatoid arthritis. In children and young adults — usually between the ages of 16 and 40 — it’s called young-onset rheumatoid arthritis (YORA). In people who develop symptoms after they turn 60, it’s called later-onset rheumatoid arthritis (LORA).
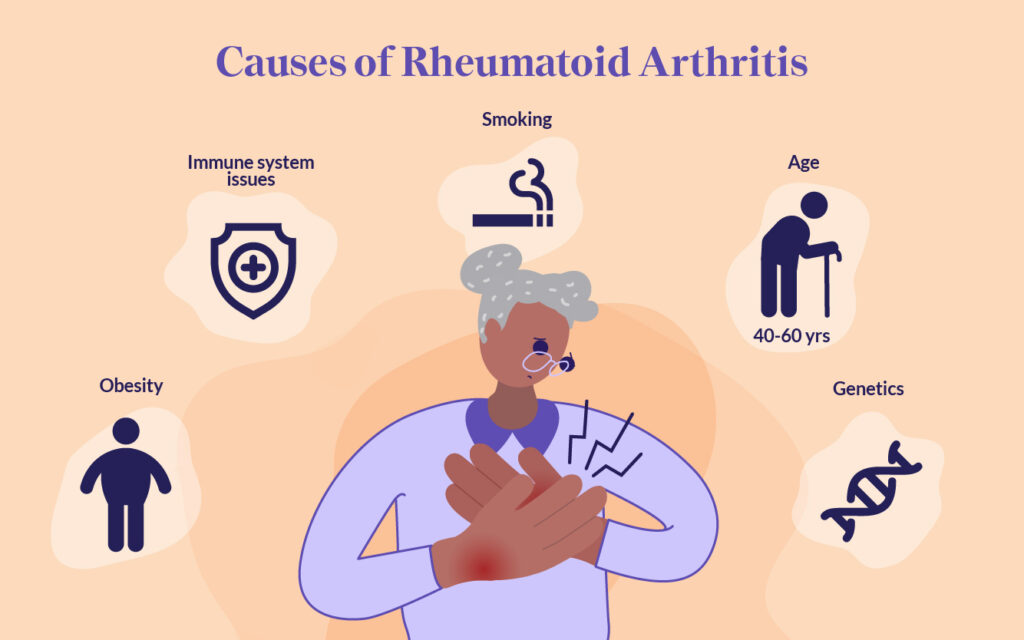
Causes for RA
In a healthy person, the immune system fights invaders, such as bacteria and viruses. With an autoimmune disease like RA, the immune system mistakes the body’s cells for foreign invaders and releases inflammatory chemicals that attack those cells. Tn RA, it attacks the synovium, the tissue lining around a joint that produces a fluid to help the joint move smoothly. The inflamed synovium gets thicker and makes the joint area feel painful and tender and look red and swollen, and moving the joint may be difficult. Some other causes include smoking, Obesity and Age too.
Symptoms for Rheumatoid Arthritis
In the early stages, people with RA may not see redness or swelling in the joints, but they may experience tenderness and pain.
These symptoms are clues to RA:
- Joint pain, tenderness, swelling or stiffness that lasts for six weeks or longer.
- Morning stiffness that lasts for 30 minutes or longer.
- More than one joint is affected.
- Small joints (wrists, certain joints in the hands and feet) are typically affected first.
- The same joints on both sides of the body are affected.
Many people with RA get very tired (fatigue) and some may have a low-grade fever. RA symptoms may come and go. Having a lot of inflammation and other symptoms is called a flare. A flare can last for days or months
Diagnosis
Rheumatologists diagnose people with rheumatoid arthritis based on a combination of several factors. Doctors do a physical exam and ask you about your medical history and symptoms. Your rheumatologist will order blood tests and imaging tests.
The blood tests look for inflammation and blood proteins (antibodies) that are signs of rheumatoid arthritis. These may include:
- Erythrocyte sedimentation rate (ESR) or “sed rate” confirms inflammation in your joints.
- C-reactive protein (CRP).
- About 80% of people with RA test positive for rheumatoid factor (RF).
Some of the imaging tests to diagnose bone health may include:
- X-rays.
- Ultrasounds.
- Magnetic resonance imaging (MRI) scans.
What are the diagnostic criteria for rheumatoid arthritis?
- Inflammatory arthritis in two or more large joints (shoulders, elbows, hips, knees and ankles).
- Inflammatory arthritis in smaller joints.
- Positive biomarker tests like rheumatoid factor (RF) or CCP antibodies.
- Elevated levels of CRP or an elevated sed rate.
- Your symptoms have lasted more than six weeks.
Health Effects
- Eyes – Dryness, pain, inflammation, redness, sensitivity to light and trouble seeing properly.
- Mouth – Dryness and gum inflammation, irritation or infection.
- Skin – Rheumatoid nodules — small lumps under the skin over bony areas.
- Lungs – Inflammation and scarring that can lead to shortness of breath and lung disease.
- Blood vessel – Inflammation of blood vessels that can lead to damage in the nerves, skin and other organs.
- Blood – A lower than normal number of red blood cells.
- Heart – Inflammation can damage the heart muscle and the surrounding areas.
- Painful joints also make it hard to exercise, leading to weight gain. Being overweight may make people with RA more likely to develop high cholesterol, diabetes, heart disease and high blood pressure.
MANAGEMENT AND TREATMENT
What are the goals of treating rheumatoid arthritis?
The goals of RA treatment are to:
- Stop inflammation or reduce it to the lowest possible level (put disease in remission).
- Relieve symptoms.
- Prevent joint and organ damage.
- Improve function and overall well-being.
- Reduce long-term complications.
How is rheumatoid arthritis treated?
Joint damage generally occurs within the first two years of diagnosis, so it’s important to see your provider if you notice symptoms. Treating rheumatoid arthritis in this “window of opportunity” can help prevent long-term consequences.
Treatments for rheumatoid arthritis include lifestyle changes, therapies, medicine and surgery. Your provider considers your age, health, medical history and how bad your symptoms are when deciding on a treatment.
Will changing my diet help my rheumatoid arthritis?
When combined with the treatments and medications your provider recommends, changes in diet may help reduce inflammation and other symptoms of RA. But it won’t cure you. You can talk with your doctor about adding good fats and minimizing bad fats, salt and processed carbohydrates. No herbal or nutritional supplements, like collagen, can cure rheumatoid arthritis. These dietary changes are safer and most successful when monitored by your rheumatologist.
But there are lifestyle changes you can make that may help relieve your symptoms. Your rheumatologist may recommend weight loss to reduce stress on inflamed joints.
People with rheumatoid arthritis also have a higher risk of coronary artery disease. High blood cholesterol (a risk factor for coronary artery disease) can respond to changes in diet. A nutritionist can recommend specific foods to eat or avoid to reach a desirable cholesterol level.
Four stages of rheumatoid arthritis
- Stage 1: In early stage rheumatoid arthritis, the tissue around your joint(s) is inflamed. You may have some pain and stiffness. If your provider ordered X-rays, they wouldn’t see destructive changes in your bones.
- Stage 2: The inflammation has begun to damage the cartilage in your joints. You might notice stiffness and a decreased range of motion.
- Stage 3: The inflammation is so severe that it damages your bones. You’ll have more pain, stiffness and even less range of motion than in stage 2, and you may start to see physical changes.
- Stage 4: In this stage, the inflammation stops but your joints keep getting worse. You’ll have severe pain, swelling, stiffness and loss of mobility.
Difference between
Rheumatoid arthritis vs. osteoarthritis
Rheumatoid arthritis and osteoarthritis are both common causes of pain and stiffness in joints. But they have different causes. In osteoarthritis, inflammation and injury break down your cartilage over time. In rheumatoid arthritis, your immune system attacks the lining of your joints.
Rheumatoid arthritis vs. gout
Rheumatoid arthritis and gout are both painful types of arthritis. Gout symptoms include intense pain, redness, stiffness, swelling and warmth in your big toe or other joints. In gout, uric acid crystals cause inflammation. In rheumatoid arthritis, it’s your immune system that causes joint damage.
GENERAL DIETARY GUIDELINES FOR RHEUMATOID ARTHRITIS
Food Items To Limit – The food stuff that limits calcium absorption should be limited.
- Phytates: They easily bind to calcium therefore limiting its availability for absorption. Try not to eat phytate-containing foods like whole wheat, oats, and rice,black beans,kidney beans, soy beans, peanuts, and lentils, walnuts, almonds, and sesame seeds, potatoes, turnips, beets and carrots with dairy products.
- Oxalates: Found in sweet potatoes, spinach and beetroot. Very reactive molecules. Bind to calcium therefore reducing its absorption. Interfere with calcium storage in cells. Don’t eliminate these foods, just be aware that they are not the best providers of calcium.
- Alcohol: Interferes with vitamin D activation by the liver and kidneys. Inhibits vitamin D activating enzymes in the liver. It is a diuretic therefore it increases calcium excretion through urine. Increases Parathyroid hormone (PTH) levels and therefore decreases calcium reserves in the body. Try to limit your alcohol intake.
- Caffeine: It is believed that caffeine decreases calcium absorption by interfering with vitamin D absorption. Caffeine is also a diuretic therefore it increases calcium excretion in the urine.
Do’s:
- Include high calcium rich foods (beans, milk, cheese, tofu, fish, dry fruits)
- Eat fresh, alkalizing vegetables and fruits every day, preferably organic like green leafy vegetables, Cruciferous vegetables, Olives, Onion, Garlic and all Citrus fruits like Orange, lemon, grapefruit (chakotra).
- Prefer home made foods over outside foods.
- Do check for iodine content on food labels.
- Include omega-3 rich foods such as fish, walnuts, almonds, flax seeds, olive oil, canola oil.
Don’ts
- Avoid consumption of caffeinated products.
- Limit the intake of phosphorus containing foods- red meat, soft drinks. Never consume Iron rich foods along with calcium rich foods as that might lead to malabsorption.
- Foods with high levels of oxalic acid such as spinach, collard greens, and sweet potatoes prevent calcium absorption. So don’t consume calcium rich foods along with these foods.
- Don’t smoke – RA is probably caused by a combination of the genes you are born with and certain events in your life that trigger those genes to become active. One of those triggers may be smoking.
- Don’t be a couch potato – Unless your joints are very inflamed, you need to get up and exercise. Studies show that aerobic and strengthening exercises can help reduce the pain and stiffness of RA.
- Don’t drink alcohol – if you are taking RA medications before checking with your doctor. Although moderate drinking may have some health benefits for people with RA, certain RA medications do not mix well with alcohol. These include the common RA drug methotrexate and nonsteroidal anti-inflammatory drugs (NSAIDs).
- Don’t spend all your time indoors – Your body needs Vitamin D
- Don’t take fish oil supplements before checking with your doctor. There is some evidence that the omega-3 fatty acids found in coldwater fish may be good for people with RA. Eating fish is fine, but taking high doses of supplements could interfere with several common medications and cause dangerous side effects.
Food Items You Can Easily Consume in Rheumatoid Arthritis
- Cereals & cereal products: Ragi, bajra, whole wheat flour. Pulses & Legumes: Lentils, peas, kidney beans, chickpeas, toor daal, soy beans.
- Fruits & Vegetables: Custard apples, chikoos, apple, white jamun, grapes, lemons, oranges, raw mangoes, carrots, beetroots, bottle gourd, bitter gourds, spinach, colocasia (arbi), drumsticks, yam, taro, tapioca, coriander leaves, celery, spring onions, garlic, ginger.
- Milk & milk products: Milk liquid, curd, cottage cheese, ghee, chhach, lassi, custard.
- Meat, Fish & Poultry: Sweet and salt water fishes, eggs, Chicken (lean and/or fowl).
- Nuts & Oils: Almonds, raisins, pista, walnuts, vegetable oil, mustard oil.
- Milk products, yogurt etc.,
For more information click here
If you are struggling shedding weight. You can talk to us by taking this assessment: Click here